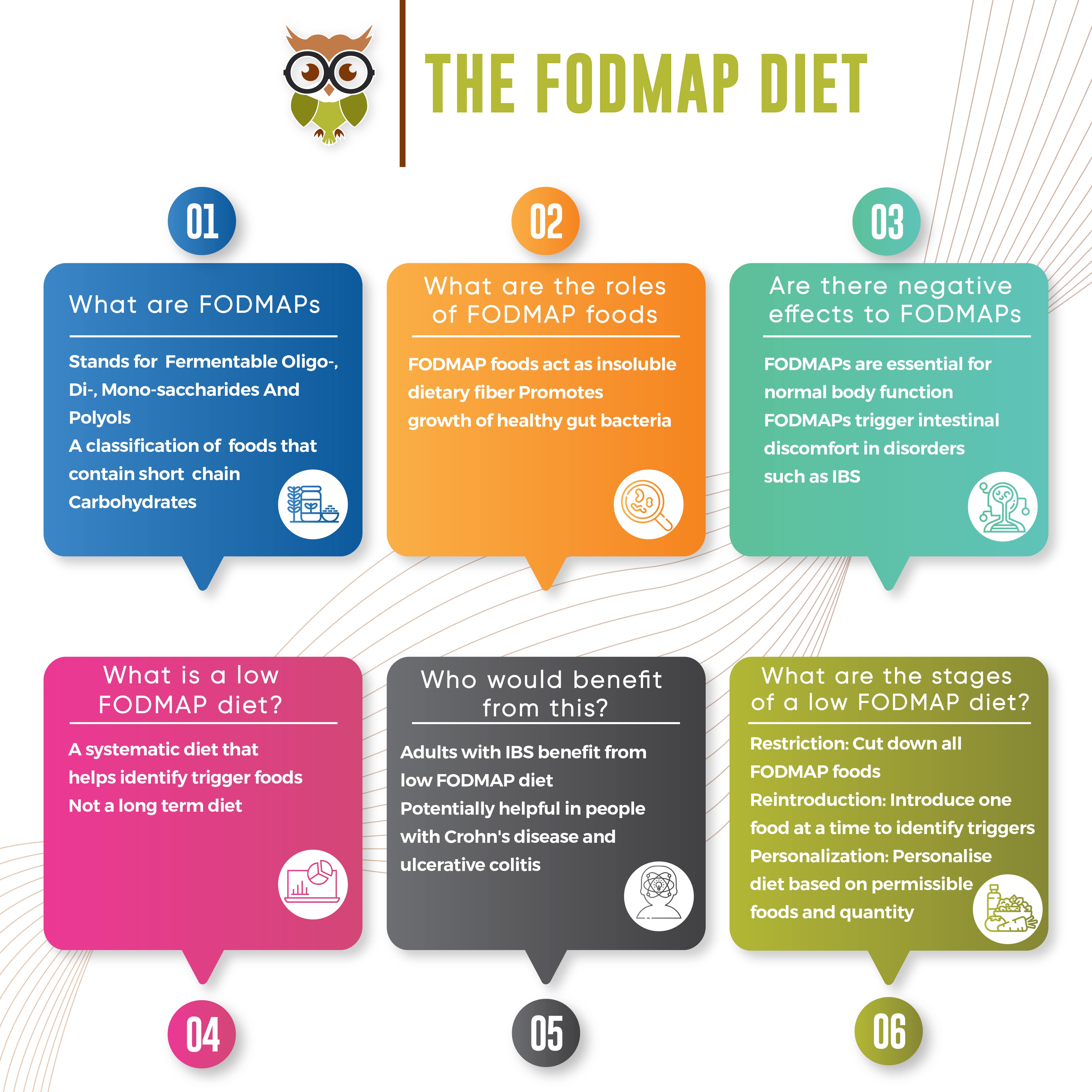
The FODMAP Diet
In a recent article about Irritable Bowel Syndrome, I had spoken about the advantages of following a low FODMAP diet to help ease the condition. I thought it would be helpful to delve deeper into the subject of what FODMAPs are and how following a low FODMAP diet can help few people.
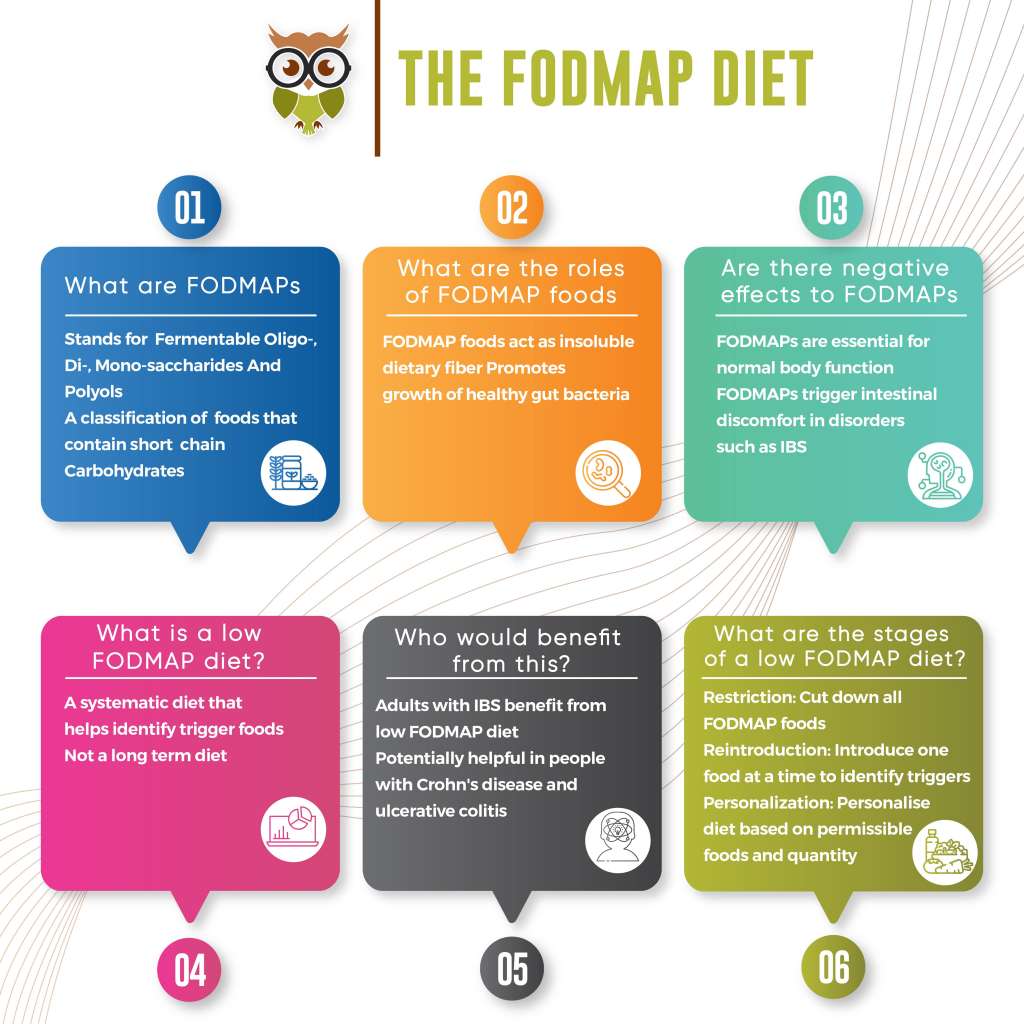
What are FODMAPs?
FODMAP is an acronym that stands for Fermentable Oligo-, Di-, Mono-saccharides And Polyols. It’s a fancy name for scientific classification of certain food groups that contain short chain carbohydrates. A few examples of these short chain carbohydrates are:
Oligosaccharides(More than 2 Carbs joined together): Wheat, rye, legumes and various fruits and vegetables, such as garlic and onions.
Disaccharides(2 Carbs joined together): Milk, yogurt and soft cheese. Lactose is the main carb.
Monosaccharides(Single Carb molecules): Various fruit including figs and mangoes, and sweeteners such as honey and agave nectar. Fructose is the main carb.
Polyols(Sugars with hydroxyl groups in them): Certain fruits and vegetables including blackberries and lychee, as well as some low-calorie sweeteners like those in sugar-free gum.
What are the roles of FODMAP in the gut?
FODMAPs are found in a majority of food groups in varying concentrations and play an essential role in gut health. They are classified as prebiotic foods that boost the growth of healthy gut bacteria. Even in individuals without any intestinal discomfort, FODMAP foods are poorly digested and passed out in the stool. The friendly gut bacteria use these foods as fuel producing methane as a by-product. They are essentially what would constitute the dietary fiber in your diet.
While the FODMAPs play an essential role in a normal individual, they tend to cause discomfort in individuals with gastrointestinal issues such as IBS. In such individuals, the undigested FODMAPs tend to move into the colon where bacteria use up the food as fuel and produce hydrogen gas a by-product leading to symptoms such as gas, bloating, stomach cramps and pain. Another thing to note here is that FODMAPs are osmotically active, which means that they can draw water into your intestine and contribute to diarrhea.
What is a low FODMAP diet?
A low FODMAP diet is a process of completely eliminating foods high in FODMAPs for a period till you see an improvement in quality of life. Then there is a systematic reintroduction of FODMAP foods one at a time to identify your tolerance level for these foods and to identify trigger foods for symptoms.
A low FODMAP diet is not a long term diet or the ultimate solution to your ailments. It is an analytical process to find what works best for you to improve your quality of life.
Who would benefit from a low FODMAP diet?
A majority of the studies and research related to FODMAPs have been conducted in adults with Irritable Bowel Syndrome. A few preliminary studies have also established an advantage of following a FODMAP diet in individuals with inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis.
It is important to note that a few foods classified as FODMAPs may cause intolerances irrespective of intolerance to FODMAPs common examples of which are Lactose and Fructose intolerances.
It is thus essential to rule out all of these factors and establish that it’s absolutely essential to get on a low FODMAP diet before you start the process. As explained before, FODMAPs are essential for normal body function and restricting them unless needed could lead to adverse effects.
A doctor would recommend a FODMAP diet after eliminating all intolerances through a breath test and after ruling out most gastrointestinal disorders which can be treated by other means. In most cases, a low FODMAP diet is reported as a secondary measure when there’s no response to primary treatment methods.
How would one go about following a low FODMAP Diet?
As mentioned before, this is not a long term diet. It is a very systematic process that involves 3 stages and it’s not advisable to go about these steps without the guidance of a dietitian and/or a doctor. The stages are as follows:
Stage 1 – Restriction: This stage involves cutting out all foods high in FODMAP from your diet for a period of 3 – 8 weeks depending on how long it takes for symptoms to disappear. While a few people might find relief in symptoms within a week or so, some might take the entirety of 8 weeks.
If no relief in symptoms is seen after 8 weeks, the individual has to immediately stop trying out the diet as FODMAPs form an essential part of the diet and cannot be restricted for longer.
Stage 2 – Reintroduction: Once the symptoms have subsided, the next step is to reintroduce FODMAP rich foods one at a time for a period of ~3 days each. The aim of this step is to identify what FODMAPs you are able to tolerate and how much of it you can tolerate.
Stage 3 – Personalization: The final stage involves taking information from the Reintroduction stage to personalize and tailor the list and amount of FODMAP foods you can consume without triggering any symptoms of discomfort.
Where can I find a list of FODMAP foods?
Although a majority of FODMAP food lists are available online, the most comprehensive list of FODMAP foods is maintained by King’s College London and Monash University.
What’s the Bottom Line?
FODMAP foods form an essential part of an individual’s diet. They constitute to the dietary fiber of an individual’s diet and boost the growth of good gut bacteria. Avoiding FODMAPs completely is close to impossible to do as a huge variety of foods contain them in varying concentrations and doing so would also have adverse effects. But in individuals with certain gastrointestinal disorders such as IBS would be able to lead a better quality of life if they are able to identify their trigger FODMAP foods and avoid them. It is also essential to have this as a last resort and go through the process with the guidance of a doctor and a dietitian.
References
- Barrett, J. S., & Gibson, P. R. (2012). Fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAPs) and nonallergic food intolerance: FODMAPs or food chemicals? Therapeutic Advances in Gastroenterology, 5(4), 261–268. doi: 10.1177/1756283×11436241
- Ong, D. K., Mitchell, S. B., Barrett, J. S., Shepherd, S. J., Irving, P. M., Biesiekierski, J. R., … Muir, J. G. (2010). Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. Journal of Gastroenterology and Hepatology, 25(8), 1366–1373. doi: 10.1111/j.1440-1746.2010.06370.x
- Staudacher, H. M., Whelan, K., Irving, P. M., & Lomer, M. C. E. (2011). Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. Journal of Human Nutrition and Dietetics, 24(5), 487–495. doi: 10.1111/j.1365-277x.2011.01162.x
- A Diet Low in FODMAPs Reduces Symptoms of Irritable Bowel Syndrome. Halmos, Emma P. et al. Gastroenterology, Volume 146, Issue 1, 67 – 75.e5