Diabetes 101: We’ve got the Deets!
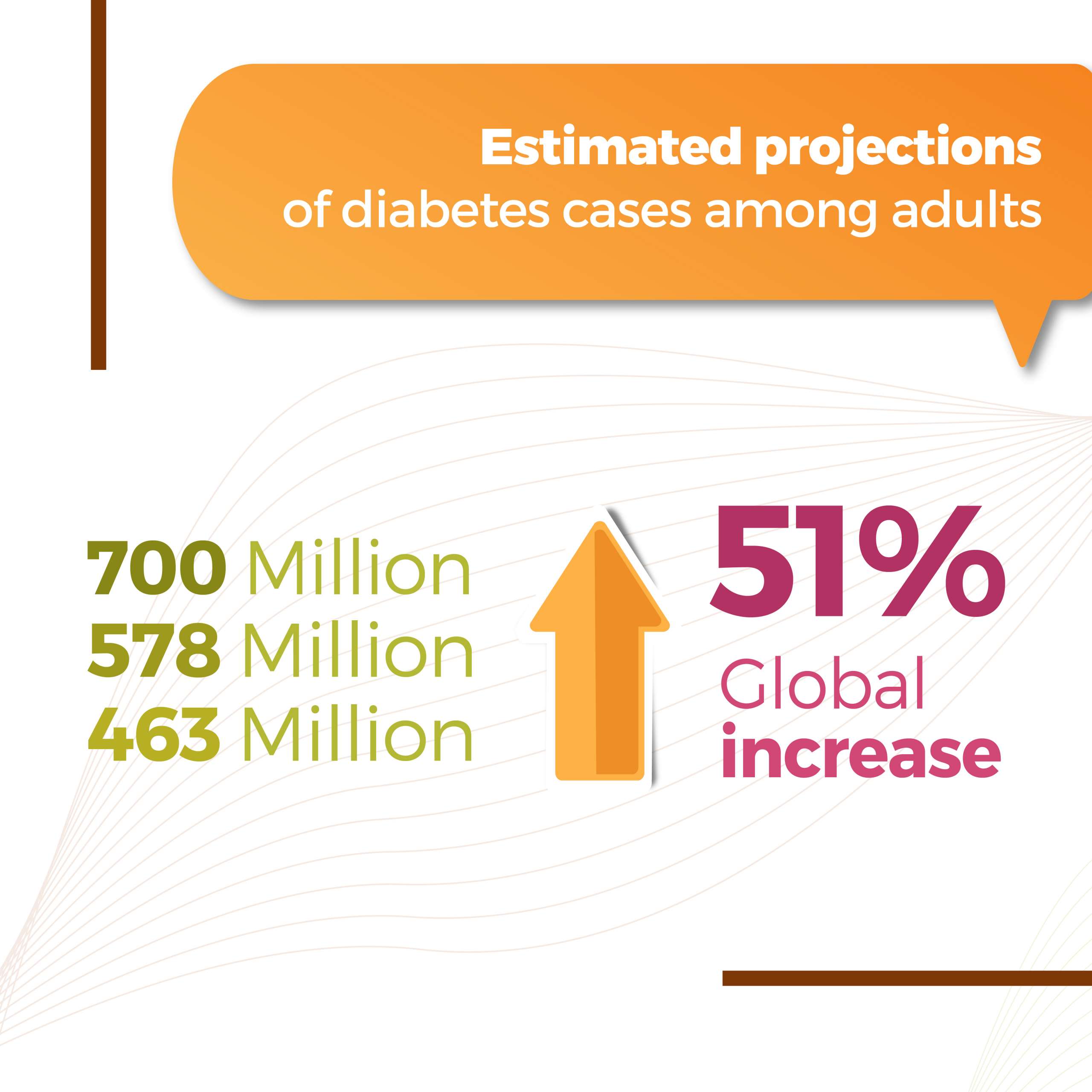
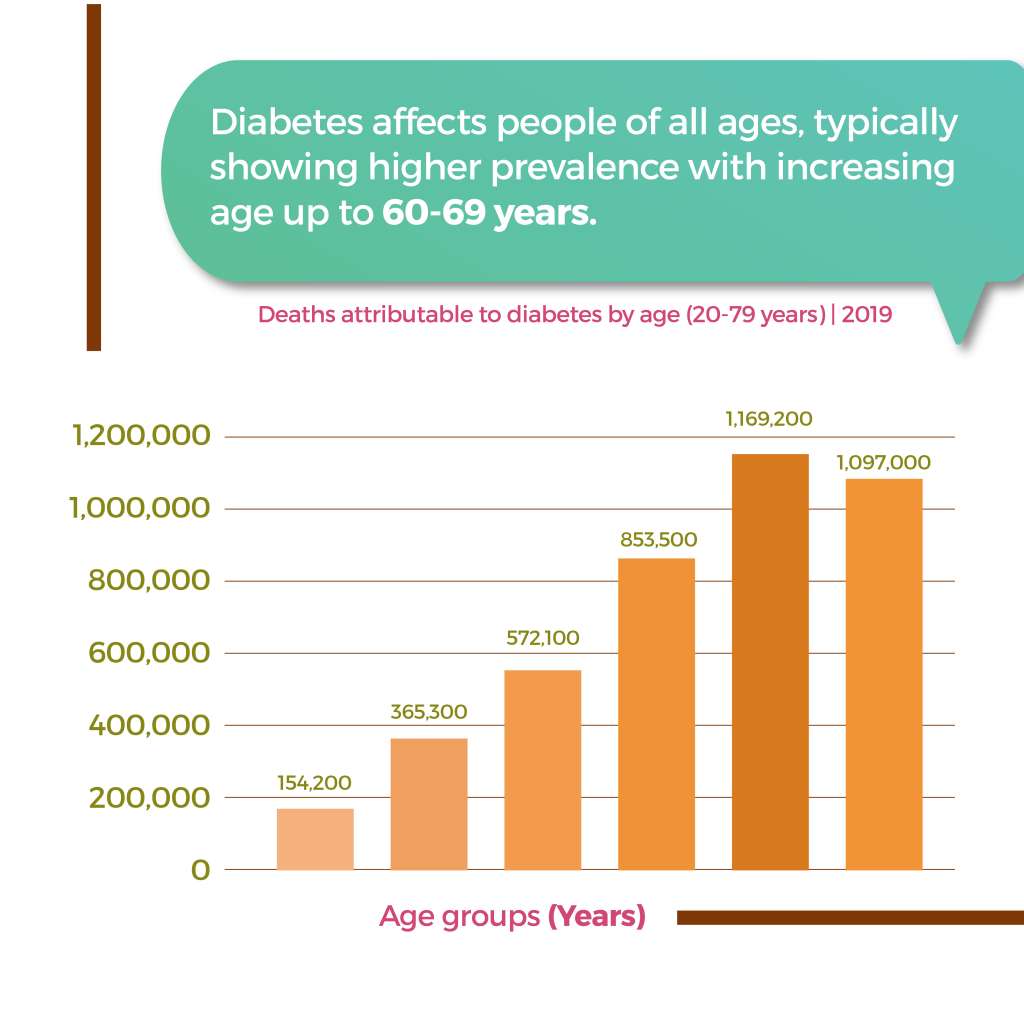
One of the disorders that’s now a household name, Diabetes has certainly had a global impact in the recent years. With data showing alarming future projections of diabetes cases across the world, let’s first understand this disorder in its entirety.

Let’s get real, folks: “A touch of sugar” does not create diabetes. Even sugar consumption cannot cause diabetes on its own. But let’s find out what does:
The deciding factor is insulin. If your body cannot make any, you have type 1 diabetes; if your body doesn’t utilise or make insulin, you have type 2 diabetes. The former is irreversible and lifelong care is required. Type 2 diabetes is majorly a lifestyle disorder which can be managed and in most cases, reversed.

Now that we’ve understood the role insulin plays in our bodies, let’s narrow down on what happens when there’s an insulin resistance. When you consume food, the digestion does its job and breaks it down to glucose. Now since insulin cannot grab the glucose from the bloodstream, the excess remains and elevates your blood glucose levels.
| So how do you know whether you have diabetes or not? Your biomarkers confirm them. When testing for diabetes, the main parameters one checks are fasting blood sugar, post-prandial blood sugar, HbA1c, HOMA-IR and urinary glucose levels. |
Does nutrition have an impact on insulin resistance?
It most certainly does. The how, is still in the works. Even in the scientific world there’s a heated discussion on which nutrition guidelines have a sustainable effect on reversing and/or managing diabetes. Is it the macronutrient composition or the energy activity? How does one examine evidence from previously conducted trials? Is there a truly sustainable method of eating that can without-a-doubt reverse type 2 diabetes?
Rest easy, we’ve got the facts compiled for you.
There has been a degree of consensus in these areas…
A priority is Weight Management, since weight loss goes hand-in-hand with improvements in glycemia, blood pressure and lipids. Maintaining the required Energy Balance is another, where guidelines recommend portion control along with physical activity. Evidence-based Dietary Patterns such as higher intake of vegetables, fruit, whole grains, nuts, legumes and yoghurt, tailored to the individual. Certain Foods to Avoid or reduce include processed red meats, refined grains and sugars for prevention and management of type 2 diabetes.
Whereas in these areas, there remains uncertainty in guidelines…
An issue most contentious in type 2 diabetes management is the optimal macronutrient composition, with variations among countries, nutritionists and those with diabetes themselves. While fish intake is recommended to manage cardiovascular risks, there’s a spectrum of association with diabetes: positive, negative or none at all! There has been consistent beneficiary evidence on yoghurt but other dairy products have yet to be conclusively examined. Oils and which type is preferable is still debated, though olive oil has shown evidence of potential benefits.
So what exactly does a person with diabetes eat?
Well, therein lies the work. Those with diabetes have had a multitude of diet options thrown at them: paleo, keto, vegan and more. The fact remains that a ‘standardised diet’ does not work in the long term, period. Within the existing nutrition guidelines, one must craft a personalized meal plan based on their food preferences, lifestyle conditions and environment. Do remember that nutrition is an evolving process, it is advisable for those with diabetes to consult a nutritionist before making drastic nutritional shifts.
| Among the plethora of studies undertaken, the Mediterranean diet has attracted multiple diabetes trials. A 12-month trial found that participants on a low carb Mediterranean diet demonstrated greater weight loss, improved glycemic and HDL levels! However studies have yet to conclude if the same will continue in the long run. |
Okay, but is exercise really that necessary?
Exercise is recommended for people regardless of any disorders. Those with diabetes are particularly encouraged to exercise to improve cardiovascular and overall fitness, weight control and to enhance their quality of life. Exercise and resistance training may benefit and improve glycemic control.
Did you know that the type and timing of your meals impact your blood glucose responses to exercise? People with diabetes and insulin dosages have to ensure that their insulin levels and carbohydrate intake are coordinated to reduce hypoglycemia. Care has to be taken with pre-workout and post-workout meals – consuming the appropriate quantity of carbs in accordance with blood glucose levels.
So with exercise and nutrition in check, can type 2 diabetes be reversed?
Although once considered irreversible and progressive, recent years have seen a shift in management and reversal of type 2 diabetes. Despite this, there is little evidence on the sustainability and lasting effect of such reversal and the potential for remission. The question of the hour is which plays a more predominant role in achieving remission: energy deficit or macronutrient composition. For more on this, keep an eye out for our next blog post in this series.
Until we meet again,
![]()