PCOD/PCOS.
This term is commonly heard of nowadays. We see several women diagnosed with this condition. But what is it? Do we really know?
This article aims to cover the basics of Polycystic Ovarian Syndrome (PCOS) or Polycystic Ovarian Disease (PCOD). We believe it is imperative to have basic knowledge about the conditions that are seen today and make ourselves more aware.
What is PCOS?
Polycystic Ovarian Syndrome, commonly known as PCOS is a metabolic, endocrine and reproductive disorder seen in women of reproductive age (1,2). It is characterised by a myriad of signs and symptoms associated with ovarian dysfunction and androgen excess (1,2). The signs and symptoms associated with PCOS varies from person to person, and will be discussed in the coming section.

Why does it occur?
The exact cause for PCOS remains mostly unknown. It is said to be a multifaceted disease (1) in which a variety of factors play a role in the development. These include environmental and/or genetic influence, diet, lifestyle, ovarian steroidogenesis, abnormal insulin signalling and excess oxidative stress. (1,2).
What are the signs and symptoms?
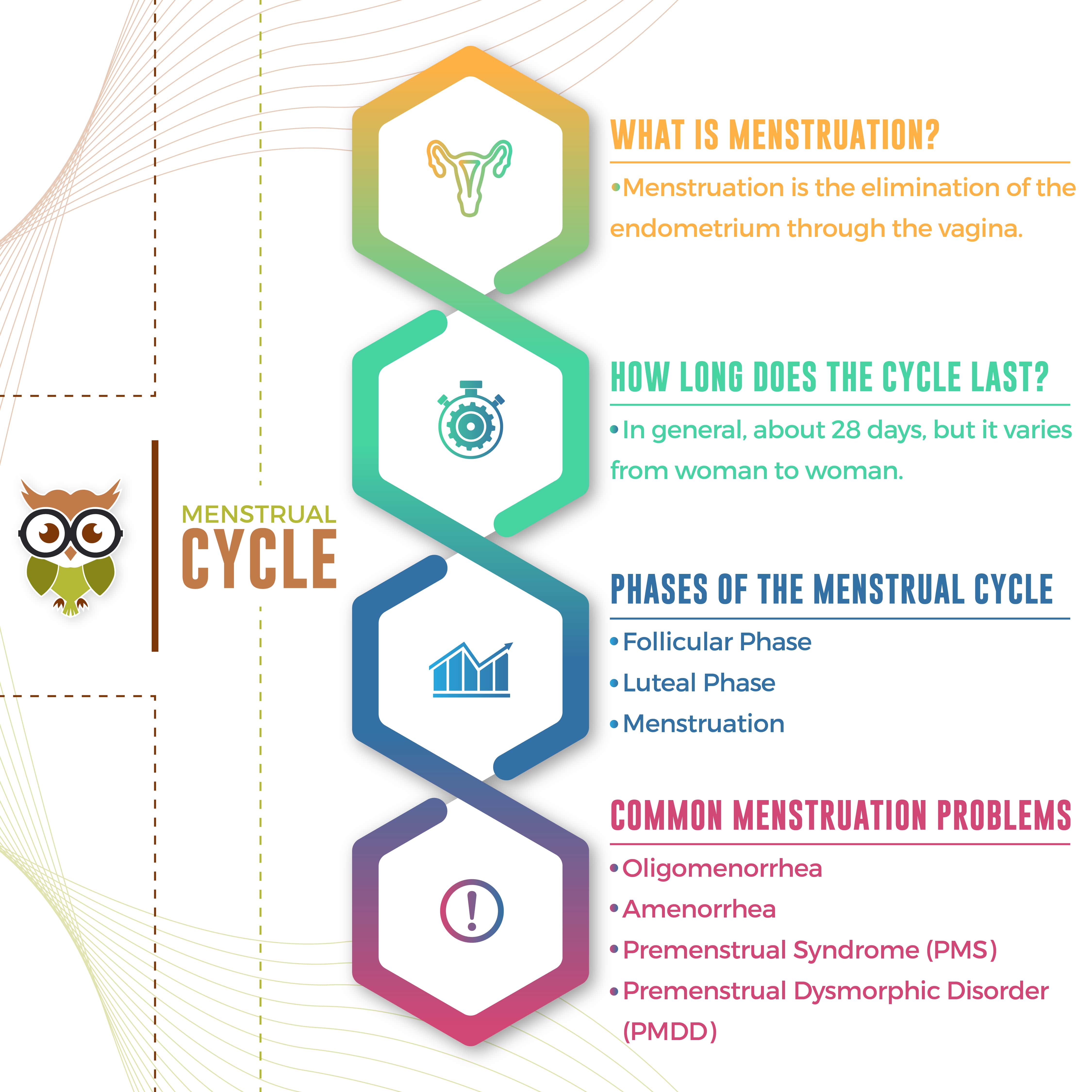
As mentioned earlier, PCOS is characterized by a variety of signs and symptoms. Any combination of these symptoms could indicate the possibility of PCOS. Menstrual irregularities, obesity or excess androgen could be a sign of this disease. However, in order to standardise the signs and symptoms, the Rotterdam Criteria is used as a rule of thumb (3). The presence of any two of the three symptoms listed in Table 1 are used to diagnose the presence of PCOS. (3,1) To confirm the presence of polycystic ovaries, an ultrasound is performed by the gynaecologist.
However, it is to note that although widely used, the Rotterdam criteria for diagnosing PCOS has been questioned due to a paucity in data (4).
In addition a fasting lipid panel, BMI, waist circumference a 2-h glucose challenge test must be done (4,5). Also, screening for thyroid disorders is important as thyroid disorders are a common cause of menstrual irregularity (5).
Table 1: Signs and symptoms associated with PCOS.
| Hyperandrogenism | Hirsutism Acne Androgenetic Alopecia Acanthosis Nigricans High circulating testosterone and androstenedione |
| Menstrual Irregularity | Oligomenorrhea (infrequent menstruation) Amenorrhea (absence of menstrual cycle) High circulating Luteinizing Hormone levels |
| Polycystic Ovaries on Ultrasound | >/= 12 follicles in each ovary Follicle size between 2 and 9mm (+/- >10ml ovarian volume) |
Presence of 2 out of 3 of these symptoms are used to diagnose the presence of PCOS.
Are there different types of PCOS?
While most people assume that excess adiposity and irregular or absence of menstrual cycle is only associated with PCOS, it is imperative to know that it is not the case. As seen above, 2 out of 3 of the symptoms presented could indicate the manifestation of PCOS. Hence, it is a spectrum. Once again, the Rotterdam criteria (3) divides these into 4 phenotypes, as seen in Table 2:
| PHENOTYPE | CRITERIA |
|---|---|
| Frank or classic polycystic ovary PCOS | chronic anovulation, hyperandrogenism, and polycystic ovaries |
| Classic non-polycystic ovary PCOS | chronic anovulation, hyperandrogenism, and normal ovaries |
| Non-classic ovulatory PCOS | regular menstrual cycles, hyperandrogenism, and polycystic ovaries |
| Non-classic mild or normoandrogenic PCOS | chronic anovulation, normal androgens, and polycystic ovaries |
What are the risks?
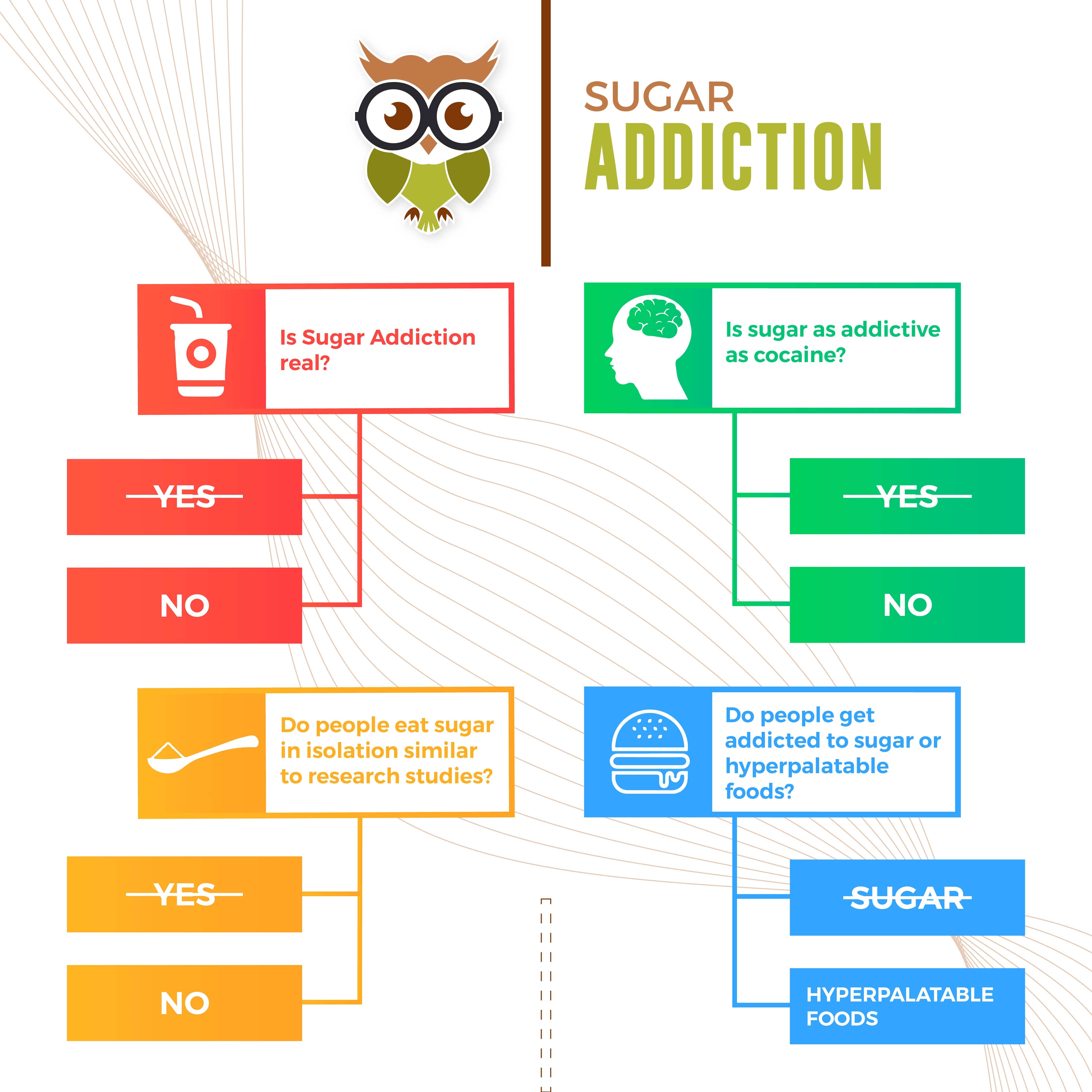
Insulin resistance (IR) is considered as an important manifestation in PCOS (6). Increased insulin and Luteinising Hormone levels could lead to anovulation (7). As a result of IR, PCOS is said to increase the risk for Type II Diabetes and gestational diabetes for the individual (8). Impaired glucose tolerance (8) and obesity are additional contributing factors to this.
Obesity is also an important feature of PCOS. However, it isn’t inherently caused by PCOS, but rather could also be due to lifestyle and environmental influences (1). Women with PCOS have more visceral fat and subcutaneous fat distribution (9). Whether obesity leads to PCOS or whether PCOS leads to obesity is still debatable (5).
Due to the nature of the symptoms women with PCOS could have a higher chance of being infertile. Infertility is more commonly associated with the existence of PCOS than healthy women (10). However, there still remains a gap in the literature on the influence of the different phenotypes on female fertility. More controlled studies are needed looking at the degree of infertility in each phenotype and the outcomes on pregnancy (1).
What is the treatment like?
Due to PCOS presenting itself as a spectrum, there is no single universal treatment. Most treatments are symptom based, targeting the issues pertaining to androgen excess,insulin resistance, hirsutism, acne and oligoovulation (1,2). In addition, lifestyle counselling should be provided in all cases in order to prevent or treat obesity (2).
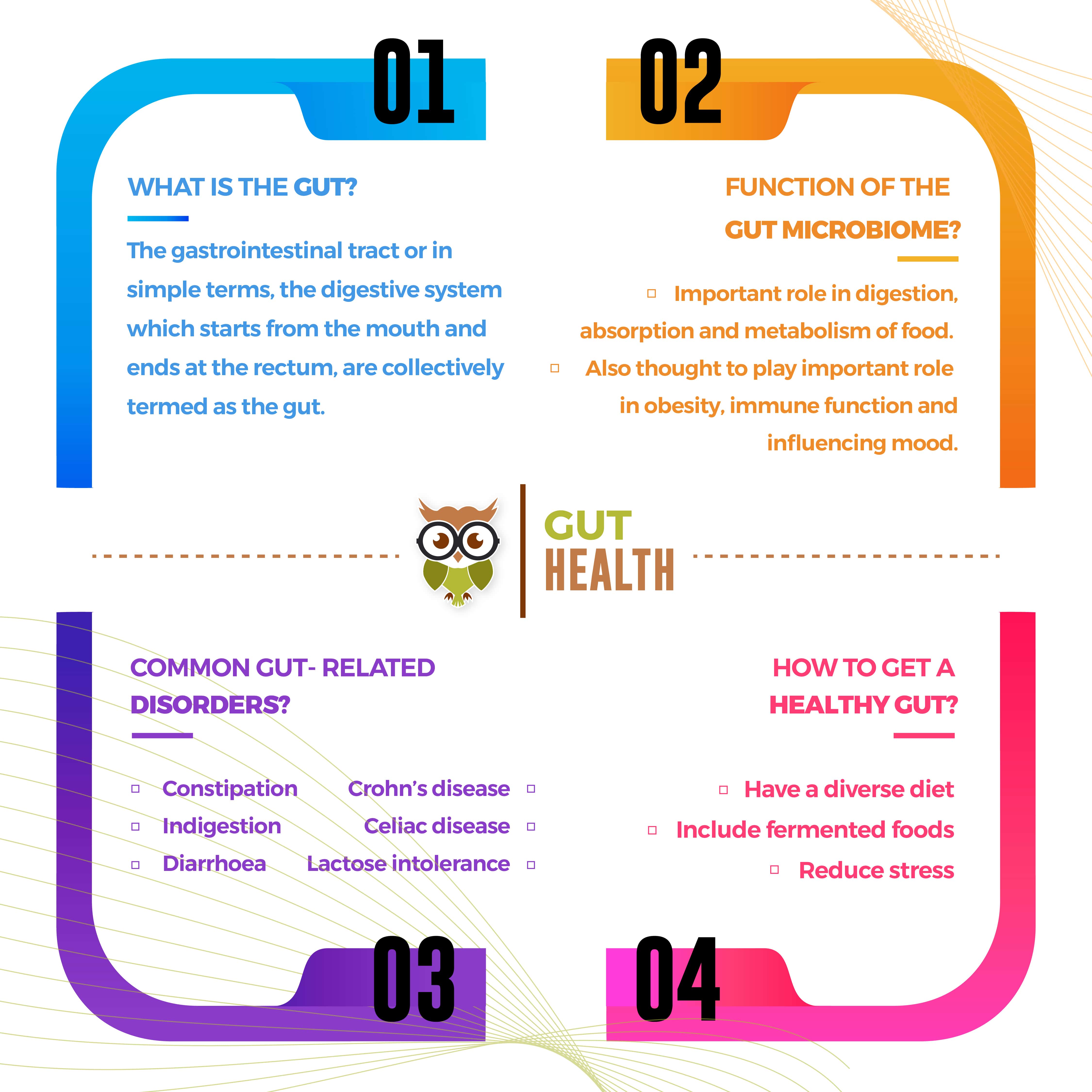
Women with Classic PCOS symptoms are likely to resume their cycles on dietary and lifestyle interventions. Dietary interventions such as consuming high fibre and protein rich foods can help with weight loss in those with PCOS. Infact, a recent review addressing nutritional management of PCOS (11) concluded that the diet composition of those with PCOS should be low in saturated fat and contain sufficient fibre from whole grains, legumes, fruits and vegetables. In addition, consumption of carbohydrates with a low glycaemic index was recommended. Soy protein has also been to have favourable effects on BMI, glycaemic control and triglycerides in those with PCOS (12)
Oral Contraceptive Pills (OCPs) are commonly used to address menstrual irregularities and hyperandrogenism (2). This helps in reducing the secretion of luteinizing hormone and decrease free testosterone levels (Costello 2007). Metformin, is another anti-diabetic drug that is used to target insulin sensitivity. Though studies using Metformin show mixed results, it is used in pregnancy complications in women with PCOS (2). However, using OCPs does have certain side effects such as mood swings, weight gain, nausea and bloating among others (13). This also varies with the dosage and type of hormone in the OCP.
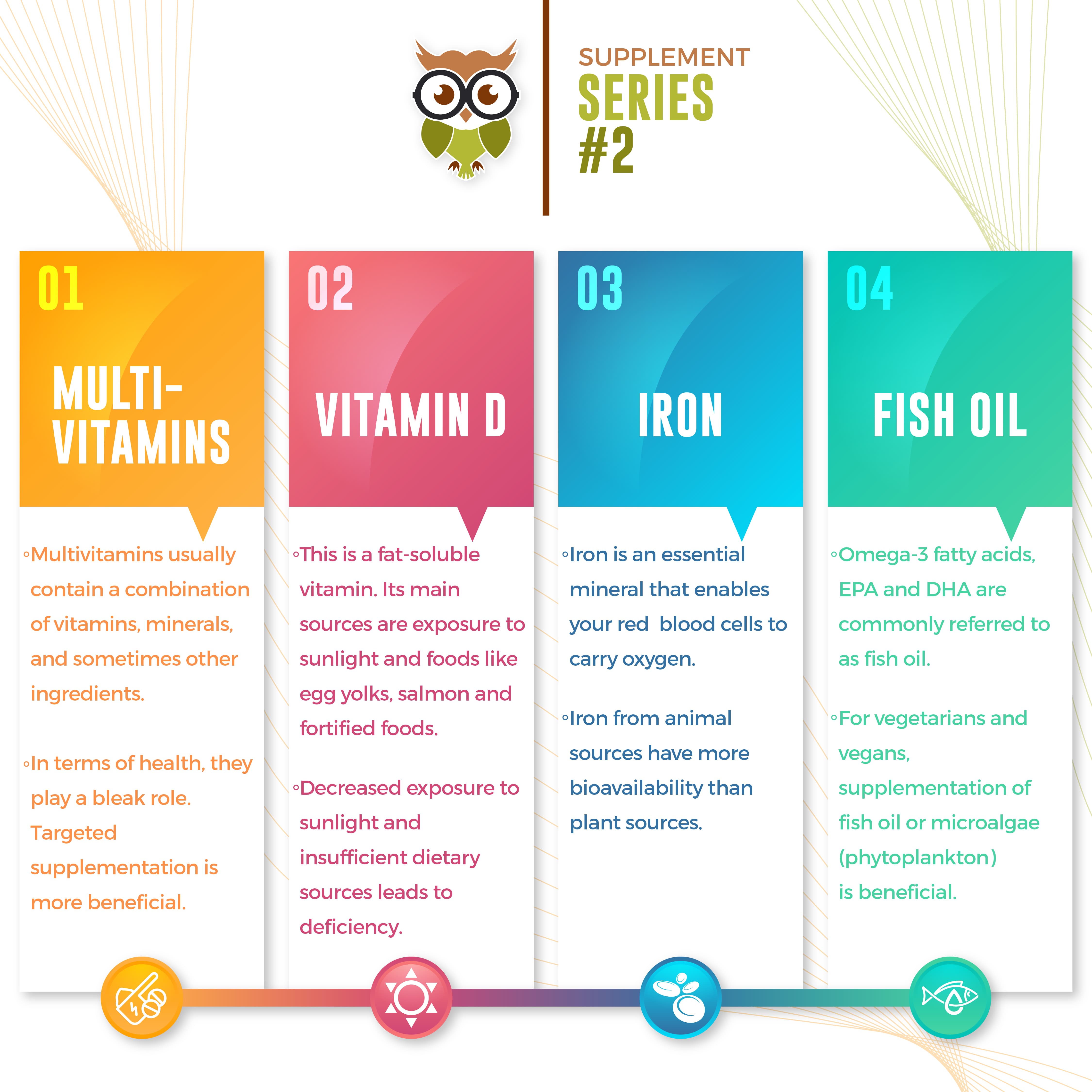
Inositol is a recent development in PCOS treatment. It is marketed as Myo-inositol (MYO) and D-chiroinositol (DCI). MYO has shown to improve insulin resistance in those with PCOS. Infact, a recent meta-analysis concluded that MYO supplementation may be beneficial in improving the metabolic profile of women with PCOS (14).
While the exact cause for PCOS is unknown, it has affected a number of women globally. It is crucial to not let this go undiagnosed. Moreover, it is also important to seek treatment from professionals. It is clear that PCOS is a multifaceted disease,that needs both medical and lifestyle interventions. There are a wide variety of treatment options available. Thus,it is not something to be feared, rather something that needs your attention.
References:
1) El Hayek S, Bitar L, Hamdar L, Mirza F, Daoud G. Polycystic Ovarian Syndrome: An Updated Overview. Frontiers in Physiology. 2016;7(124).
2) Escobar-Morreale H. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nature Reviews Endocrinology. 2018;14(5):270-284.
3)Rotterdam, E. A.-S. P. C. W. G. (2004) Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertility and Sterility. 2004;81(1):19-25.
4) Azziz R. Diagnosis of Polycystic Ovarian Syndrome: The Rotterdam Criteria Are Premature. The Journal of Clinical Endocrinology & Metabolism. 2006;91(3):781-785.
5) Kamangar F, Okhovat J, Schmidt T, Beshay A, Pasch L, Cedars M et al. Polycystic Ovary Syndrome: Special Diagnostic and Therapeutic Considerations for Children. Pediatric Dermatology. 2015;32(5):571-578.
6) Sıklar Z, Berberoğlu M, Çamtosun E, Kocaay P. Diagnostic Characteristics and Metabolic Risk Factors of Cases with Polycystic Ovary Syndrome during Adolescence. Journal of Pediatric and Adolescent Gynecology. 2015;28(2):78-83.
7) Dunaif A. Hyperandrogenic anovulation (PCOS): A unique disorder of insulin action associated with an increased risk of non-insulin-dependent diabetes mellitus. The American Journal of Medicine. 1995;98(1):S33-S39.
8)Randeva H, Tan B, Weickert M, Lois K, Nestler J, Sattar N et al. Cardiometabolic Aspects of the Polycystic Ovary Syndrome. Endocrine Reviews. 2012;33(5):812-841.
9) KIRSCHNER M, SAMOJLIK E, DREJKA M, SZMAL E, SCHNEIDER G, ERTEL N. Androgen-Estrogen Metabolism in Women with Upper BodyVersusLower Body Obesity*. The Journal of Clinical Endocrinology & Metabolism. 1990;70(2):473-479.
10) Hart R, Doherty D. The Potential Implications of a PCOS Diagnosis on a Woman’s Long-Term Health Using Data Linkage. The Journal of Clinical Endocrinology & Metabolism. 2015;100(3):911-919.
11) Faghfoori Z, Fazelian S, Shadnoush M, Goodarzi R. Nutritional management in women with polycystic ovary syndrome: A review study. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2017;11:S429-S432.
12) Karamali M, Kashanian M, Alaeinasab S, Asemi Z. The effect of dietary soy intake on weight loss, glycaemic control, lipid profiles and biomarkers of inflammation and oxidative stress in women with polycystic ovary syndrome: a randomised clinical trial. Journal of Human Nutrition and Dietetics. 2018;31(4):533-543.
13) Consensus statement on the use of oral contraceptive pills in polycystic ovarian syndrome women in India. Journal of Human Reproductive Sciences. 2018;11(2):96.
14) Unfer V, Facchinetti F, Orrù B, Giordani B, Nestler J. Myo-inositol effects in women with PCOS: a meta-analysis of randomized controlled trials. Endocrine Connections. 2017;6(8):647-658.