Blood Cholesterol Levels – The what, why and how.
High cholesterol level in blood has become so common, that almost 10 million people are diagnosed with it, every year. A seemingly simple explanation for this is our sedentary lifestyle, but the issue is a little more deep rooted than just lifestyle. What makes up your plate eventually makes up your physique, and we’re here to help you sort the plate out.
What is cholesterol, really?
Cholesterol is a waxy substance that your body needs for a lot of functions, like hormone secretion, metabolism and maintaining overall health. Carried through the body by lipoproteins, cholesterol essentially helps your body maintain balance and is a good friend.
Until, there’s too much of it in your blood. Too much blood cholesterol has a lot of consequences, but first, how much is too much?
Interpreting your blood cholesterol numbers.
There are two types of cholesterol, the High-Density Lipoprotein and the Low-Density Lipoprotein, commonly referred to as the good and the bad cholesterol. HDL absorbs excess cholesterol and takes it back to the liver, while the LDL collects on the walls of blood vessels.
| Total cholesterol level | HDL | LDL | |
| Optimal | Less than 200 mg/dl | <40 mg/dl in men, <50 mg/dl in women. | <100 mg/dl |
| High | Anything over 240 mg/dl is very high | ≥130 mg/dl |
While it is true that cholesterol levels must be kept in check, neglecting cholesterols is not the way to go either. Any HDL reading below 40 mg/dl in men and 50 mg/dl is considered low, and is not advisable in the long run.
How would I know?
Symptoms for high cholesterol levels in your blood will not show as explicitly, so the risk of it being undetected until it’s serious is quite high. The only way to find out and know for sure that you have high blood cholesterol is to have it tested by a physician.
A few physical symptoms however, are fatty bumps on your skin, called xanthomas, or grayish-white rings around the corneas in your eye, called corneal arcus. These mostly develop in people who have familial hypercholesterolemia. But waiting for these symptoms might not be the wisest decision. Have your blood cholesterol levels periodically checked and keep yourself on the know.
Who’s at risk?
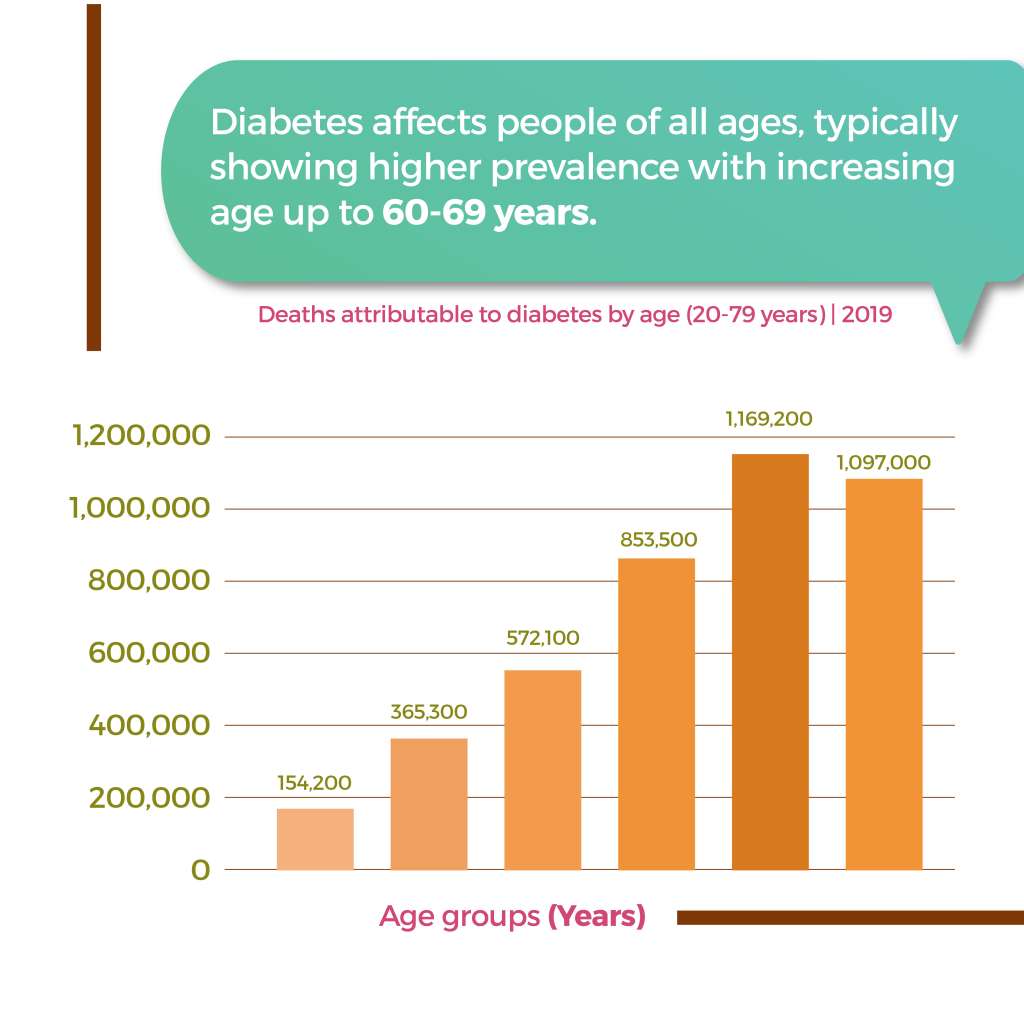
Statistically people between the ages of 40 and 59 are the ones commonly diagnosed with high blood cholesterol. Other than age, there are a few other risk factors that can increase your chances when it comes to getting diagnosed with high blood cholesterol.
As far as lifestyle choices are concerned, eating foods high in saturated fats or trans fats regularly, lack of physical activity, smoking, chronic stress and drinking too much alcohol can pose a threat. Apart from these, high blood cholesterol could also be genetic.
If you have other conditions like obesity, PCOS, Diabetes, Hypothyroidism and/or are taking medications like diuretic, steroids, or medications for chemotherapy, they might be reasons for high levels of blood cholesterol.
Dealing with it
Left unchecked for prolonged periods of time, high blood cholesterol levels can lead to serious problems, such as heart attack and stroke. So it is very important that you cope well and keep your numbers at bay.
First things first, work on what you eat. Reduce the consumption of saturated and trans fats that are found in fatty cuts of meat, dairy products, and many packaged snacks and desserts. We recommend eating fish high in omega-3 fatty acids, nuts, and the usage of certain vegetable oils such as olive oil. The DASH eating plan will help reduce your LDL, or the “bad cholesterol”.
Working on a healthier lifestyle along with a proper diet can work wonders. By healthier lifestyle we mean being physically active, keeping yourself free of too much stress, not smoking, limiting your alcohol consumption and taking the right meds when needed. Speak with your doctor and stick to the protocol, and you’ll be mighty fine!