Irritable bowel Syndrome (IBS), the functional gastrointestinal disorder, is characterized by a group of symptoms such as a change in bowel movements (diarrhea or constipation, or both), abdominal pain, bloating, and cramping.
Even though the symptoms leave no visible changes to the GI tract, if untreated – the chances of IBS aggravating are higher.
IBS is a chronic condition. People suffering from IBS are at risk of developing mental health issues since IBS can negatively affect daily life.
This blog is an attempt at understanding IBS and offers to provide a glimpse on effective every day management of this chronic disorder.
Classification of IBS
Understanding IBS is easier if we know the different categories. The board classification helps in understanding the symptoms and aids in optimizing the treatment of individuals.
IBS has four categories. Each type exhibits different symptoms.
- IBS with constipation (IBS-C) is distinguished from other IBS conditions when more than a quarter of the stools are hard or lumpy and occur for over three days in a month over the preceding three months.
- IBS with diarrhea (IBS-D): When an individual diagnosed with IBS passes more than a quarter of the stools as loose and watery, the person has IBS-D. Individuals often experience a sudden urge to use the bathroom.
- Mixed IBS (IBS-M) alternates between constipation and diarrhea. More than a quarter of the bowel movement can be hard or lumpy at one instance, and more than a quarter of the stool can be loose or water at the other. An individual can experience IBS-C and IBS-D on the same day.
- Unsubtyped IBS (IBS-U) exhibits all other symptoms associated with IBS but displays insufficient alteration of stool consistency to be classified into the subtypes mentioned above.
| IBS Type | Stool Consistency |
| IBS C | > 25% is hard or lumpy; <25% is loose or watery |
| IBS-D | >25% is loose or watery; <25% is hard or lumpy |
| IBS-M | >25% is hard or lumpy; >25% is loose or water |
| IBS-U | Insufficient alteration in the stool consistency |
Common Symptoms associated with IBS
IBS symptoms vary with individuals. The severity of the symptoms and individual might range from mild to extreme depending on food habits and lifestyle.
Each individual can have Irritable Bowel Syndrome triggering foods, eating which can trigger symptoms. Avoiding the trigger foods and changes in lifestyle can help ease the symptoms to an extent.
The common symptoms identified across individuals with IBS are:
- Abdominal pain
- Change in bowel movements
- Cramping
- Bloating
A few of the lesser-known symptoms experienced by individuals include:
- Lack of energy
- Mucus in stool
- Sudden urge to use the bathroom
- Flatulence
- The feeling of a non-empty bladder
- bowel incontinence
- Nausea or feeling sick
- Mood swings that include irritability, stress, and anxiety
As said earlier, IBS is the host of symptoms. A few of the above can also indicate other GI disorders. So, if you are experiencing a few of the above symptoms, it’s best to consult a certified practitioner for an accurate diagnosis.
Causes of Irritable Bowel Syndrome
While it’s difficult to pinpoint the exact cause of IBS, there are a few classic reasons that help explain the occurrence of IBS. Each individual may develop IBS owing to different factors.
However, in the blog, we cover a few major causes that lead to IBS.
How the brain and gut work together is one of the causes of IBS. The brain-gut interaction is essential for proper water and nutrient absorption and waste removal from the body. Alterations in this interaction disrupt the normal process, causing disorders.
- Disruptive intestinal muscle contractions can make the food move slowly or rapidly, causing changes in bowel movement. The altered gut motility changes the food retention capacity of the intestines, causing improper absorption of nutrition by the body.
- Nervous system distress acts as a trigger for IBS. Anxiety and stress can cause the brain to send an inappropriate signal to the gut inducing inappropriate bowel movements.
Other causes for IBS include:
- Infection – A bacterial infection in the digestive tract can lead to IBS. Post-infectious IBS displays one or more symptoms of fever, vomiting, diarrhea, inflammation, and positive bacterial stool culture.
- Changes in gut microbes like bacterial overgrowth in the intestine or changes in the type of bacteria in the gut disrupt the normal functioning of the GI tract, causing IBS.
Experts opine that abusive or incredibly stressful life and food sensitivity might also cause an individual to develop IBS.
Risk Factors involved in developing IBS
After extensive research into IBS, researchers have narrowed down the risk factors that lead to developing Irritable Bowel Syndrome. So, what are the risk factors, and who is at more risk of developing IBS?
- Females are at higher risk of developing IBS when compared to men.
- Age is another risk factor. People over 40 years of age are at greater risk of developing IBS. The incidence of IBS decreases with advancing age.
- A person with a family history of IBS has an increased chance of developing IBS.
- People with troubled pasts and people experiencing psychological issues like anxiety or depression are more likely to develop IBS.
- Food poisoning changes the composition of the bacterial gut and increases the chances of developing IBS.
- A few antidepressants or antibiotics can trigger IBS in an individual.
Associated comorbidities
IBS is generally associated with at least one co-morbid condition. Individuals with IBS and one or more comorbidities develop severe symptoms and experience a lower quality of life. They also experience psychological symptoms and are highly prone to develop somatization disorder.
We can broadly classify the comorbidities into three categories and present the most commonly occurring disorders in each category.
- IBS and Gastrointestinal disorders frequently occur together. Functional dyspepsia (FD) and Gastroesophageal reflux disease (GERD) are two disorders commonly seen with IBS.
- IBS overlaps with extraintestinal somatic disorders such as Fibromyalgia syndrome (FMS), Chronic fatigue syndrome (CFS), Chronic pelvic pain (CPP), sexual dysfunction, and sleep disturbances
- IBS and commonly associated psychological disorders are generalized anxiety disorder, panic disorder, major depression, and bipolar disorder
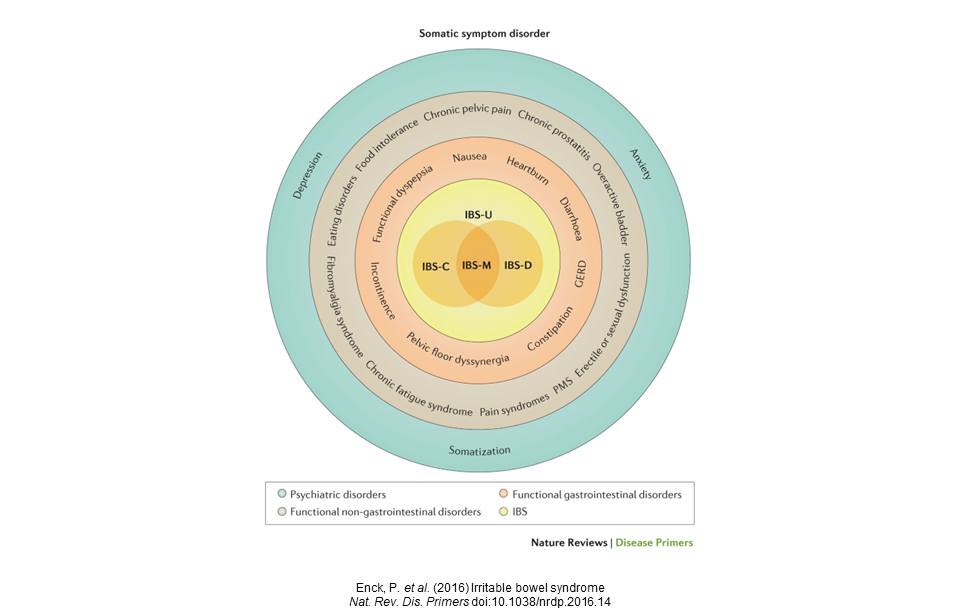
The diagram shares a more exhaustive list of IBS and associated comorbidities. Each layer adds a different complexity when treating IBS. So with comorbidities, the treatment is more about managing than treating the syndrome.
Diagnosis of IBS
Based on Rome criteria, IBS diagnosis includes identifying a pattern that involves abdominal pain or discomfort for at least three days in a month over the last three months, with the first symptom appearing at least six months before. The symptoms are:
- Changes in discomfort while passing stools
- Changes in frequency of bowel movement
- Changes in the form of the stool
So far, the diagnostic procedure involves identification by ruling out. There are no definitive tests to diagnose IBS. After collecting family history and vitals, doctors perform a physical examination and simple tests to rule out other disorders.
- Blood tests to check to rule out celiac disease, anemia, infection, and other digestive infections.
- Examine stool samples to rule out infections.
- Can perform a colonoscopy to rule out conditions like colon cancer or Inflammatory Bowel disease (IBD).
- Hydrogen breath tests to rule out digestive problems like lactose intolerance.
- Other tests for food allergies
Treatment and Management of IBS
There is no specific treatment for IBS, as the conditions and symptoms differ across individuals. One can aim to manage the symptoms by adopting a low FODMAP diet and a few lifestyle changes under the guidance of doctors or certified nutritionists.
Understanding IBS is the key to managing it effectively. Staying hydrated, exercising, managing anxiety and stress, and following a healthy diet are a few things one can try to find relief from the IBS symptoms.
A primary step in easing the symptoms is to adopt a Low FODMAP Diet. FODMAP (Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are short-chain carbohydrates that are poorly absorbed in our small intestines and can cause digestive issues.
Types of carbs that are associated with FODMAPs are:
- Fermentable oligosaccharides are fructans in wheat, rye, onion, garlic, and chicory; and food like legumes and beans contain Galatians.
- Disaccharides are lactose present in milk.
- Monosaccharides are fructose present in fruits, honey, and high-fructose corn syrup.
- Polyols are carbs in sugar alcohols, avocados, apples, cherries, stone fruit, cauliflower, mushrooms, sweeteners, etc.
What happens when you have FODMAP foods?
When a person consumes high FODMAP food, the food moves slowly through the small intestine, thereby absorbing all the water. It then reaches the large intestine, where they become the food for gut bacteria. Interaction with bacteria results in fermentation, which produces gas and causes discomfort triggering IBS or one of its symptoms.
Steps to follow the FODMAP diet for IBS:
The FODMAP diet is introduced structurally in people in three phases.
- Elimination phase: In this phase, people follow a low FODMAP diet and shun foods under a high FODMAP list over a period of 2 to 6 weeks
- Re-Introductory phase: After the successful completion of the first phase, each food in high FODMAP food is reintroduced one food at a time over three days. By increasing the serving size each day, you can monitor the tolerance over the next 8 to 12 weeks.
- Personalization phase: During the re-introductory phase, people will learn about the food best suited for them. The nutritionists devise a dietary plan for long-term sustenance based on the results obtained in the second phase.
One of the most frequently asked questions by people with IBS is: How to cure IBS permanently?
More often than not, IBS is a chronic condition that does not have a complete cure.
In case of severe symptoms, doctors prescribe medications for easing the symptoms based on the type of IBS. At a certain time, an individual might also need mental health therapies to deal with their psychological problems.
IBS is not easy to live with. One should know and learn about IBS before it leads to other complications. Talk to your doctor and find a certified nutritionist who can help you deal with Irritable Bowel Syndrome effectively.
MYTHS AND FACTS
Several myths are associated with Irritable Bowel Syndrome. Here are a few myths and facts that can help you make an informed decision.
Myth 1: IBS and IBD are the same
Fact: Though IBS and IBD (Inflammatory Bowel Disease) sound similar, they are two completely different conditions. IBD is a collective term for ulcerative colitis and Crohn’s disease, characterized by inflammation of the intestine. IBS is the improper functioning of the digestive tract.
Myth 2: Drastic Change in Diet can cure IBS
Fact: Food is not the only reason for IBS. IBS is a condition that occurs because of several factors. One can definitely ease their IBS symptoms by making the right food choices.
Myth 3: Fiber-rich food help IBS
Fact: Eating fiber-rich help with constipation but may not help with other symptoms. On the contrary, the symptoms may worsen because of the intake of fiber-rich food. So before changing your diet, consult a certified nutritionist who will guide you to eat right.
Myth 4: Fasting is a sure-shot way of curing IBS
Fact: One should not fast to cure IBS unless specified by your nutritionist. An individual with IBS should not change meal plans, food habits, and exercise regimes without expert guidance. The chances of worsening the condition are higher without proper guidance.
Myth 5: There is a prescribed diet for IBS.
Fact: The dietary pattern varies according to the symptoms and condition of the IBS in a person. There are no one-size fits all diet plans when it comes to IBS.
Myth 6: We can cure IBS by using home remedies such as ajwain or cumin seeds.
Fact: Certain home remedies, present for ages, help relieve the symptoms to an extent, but they are not the cure. IBS needs a doctor’s intervention and lifestyle changes if you are looking for proper relief from IBS.
Myth 7: Lactose intolerance and IBS are the same.
Fact: Lactose intolerance is the body’s inability to process lactose – a readily fermentable carbohydrate. While food rich in lactose can act as a trigger for IBS, IBS is a completely different condition.
Myth 8: A bad diet is the main cause of IBS
Fact: Though the symptoms surrounding IBS make it seem like food is the root cause of IBS, other factors can cause or trigger the syndrome as well. Stress, anxiety or panic attacks, hormonal imbalance, or everything together, can cause IBS. So, blaming food will not help you cure IBS.
Myth 9: Cutting down on dairy and gluten products can get rid of IBS symptoms
Fact: IBS is a chronic condition that can only be managed. For a few people sensitive to dairy products and gluten, cutting down on these trigger foods might help ease the symptoms, but this is not the case with everyone with IBS.